Could we make smell a biomarker?
What if quantifying odor could be made into a routine diagnostic parameter?
In Ali Wong’s standup special “Baby Cobra,” she had a great line that many might be too ashamed to admit. “I had to find ways to discretely scratch myself underneath the conference table, and then resist the urge to immediately smell my fingers afterwards. I want to be able to smell my fingers when I wanna smell my own goddamn fingers[.…] Nature made you urgently curious to protect you, ’cause you gotta check that it’s all good in the hood. If it’s too funky, you need to see a doctor. Your fingers are your first WebMD.” Honestly, she isn’t wrong. Check yourself before you wreck yourself - by smelling yourself.
There are many health problems where a symptom is a foul smell. Urinary tract infections (UTIs) make your pee smell like ammonia. Trimethylaminuria makes your sweat and breath smell like fish (which sounds awful to my partner, who abhors the smell of fish). Kidney and liver failure make your breath smell bad. In a lot of cases, a weird smell is our first indication that something is amiss, and that maybe it’s time to go to the doctor. But apparently, changes in body odor can also be associated with some more serious diseases. Parkinson’s disease is an example, which emits a musky odor. Isovaleric acidemia gives off a smelly feet odor, which is extremely unfortunate (unless you’re into feet, I guess. This is a no judgement blog.) And cancer can sometimes give a rotting flesh smell.
The most indicative story of the potential of smell for diagnosing disease is Joy Milne. Joy Milne has the unique ability to smell Parkinson’s disease. She detected a change in her husband’s odor that correlated with his changing personality, which eventually led to a Parkinson's disease diagnosis. When the couple started attending a Parkinson’s support group, she noticed the same smell on all the members as well. The wild thing is that the smell changed as her husband’s Parkinson’s got worse, meaning she could also smell disease progression. The story is honestly incredible and super cool. In addition to Joy, there are studies on dogs’ ability to smell cancer. There’s even a reddit thread about clinicians who can identify diseases by smell.
Other diseases change your ability to smell. Covid is an obvious one, where it made people lose their sense of smell (anosmia). Apparently, Covid can also make you have parosmia, where your sense of smell is distorted. The Cleveland clinic example of parosmia is warm cookies smelling unpleasant, which sounds absolutely horrid. Then there’s phantosmia, smelling an odor that isn’t there, which can be a symptom of neurocognitive or mood disorders. Lastly, there’s hyposmia, which is a weakened ability to smell. Besides Covid, other diseases that can alter your sense of smell include cancers, neurodegenerative diseases, traumatic brain injury, and more. It’s kind of crazy that smelling, which in my personal life I mostly use to determine if I should shower or if the food will taste good, can be such a large medical component.
Technologies to mimic olfaction
Now, if you think about it, using smell to detect things is pretty common in our society. That airport dog, sniffing you and your bags for illegal substances, is probably the most well known example of using smell to detect substances. Recently, Ronin the rat set the Guinness World Record for becoming the first rodent to sniff and detect more than 100 landmines in Cambodia. Even more cool, dogs have the ability to distinguish anxiety and stress from humans with their nose. But these animals aren’t always accurate; animals become less accurate when they are fatigued (shoutout to my old coworker Jan Steinkühler for teaching me this). So what if we could augment animals with machines to enhance their smell? Or maybe replace animals altogether with devices that can detect chemicals from smell? (animals are not unionized and so replacing them with technology shouldn’t be a problem). Digitizing this technology could have real life benefits for chemical and medical detection.
So what’s going on with the science of smell? Well, we’re starting to understand the structure of odorant receptors (ORs) and how they interact with odorants. In Class I ORs, the odorant binds at a singular position to trigger signaling, while in Class II ORs, the odorant can bind to multiple binding sites. To me, that also means that maybe Class II ORs can detect multiple types of odors. I can imagine why, evolutionarily, this responsiveness makes sense. Maybe you have a Class I ORs for dangerous smells (fire, sickly smells, waste) that are super specific. On the other hand, you might have Class II ORs for smelling delicious food. Maybe the smells thyme, rosemary, soy sauce, mint, kimchi, caramel should all activate a singular OR receptor just to tell you that the food you’re about to eat is actually seasoned (apparently, OR2W1 is pretty broad food receptor). What else? People who don’t smell breathe differently, which is and isn’t surprising. Using a wearable device to measure air flow, the authors were able to predict if a person has anosmia based on their nasal airflow patterns from healthy controls. They predict that these changes in your respiratory patterns might have contributions to health. It has been found that people with dysfunctional olfaction had 3x higher mortality rate. We knew that breathing is life, but I guess smelling is life too.
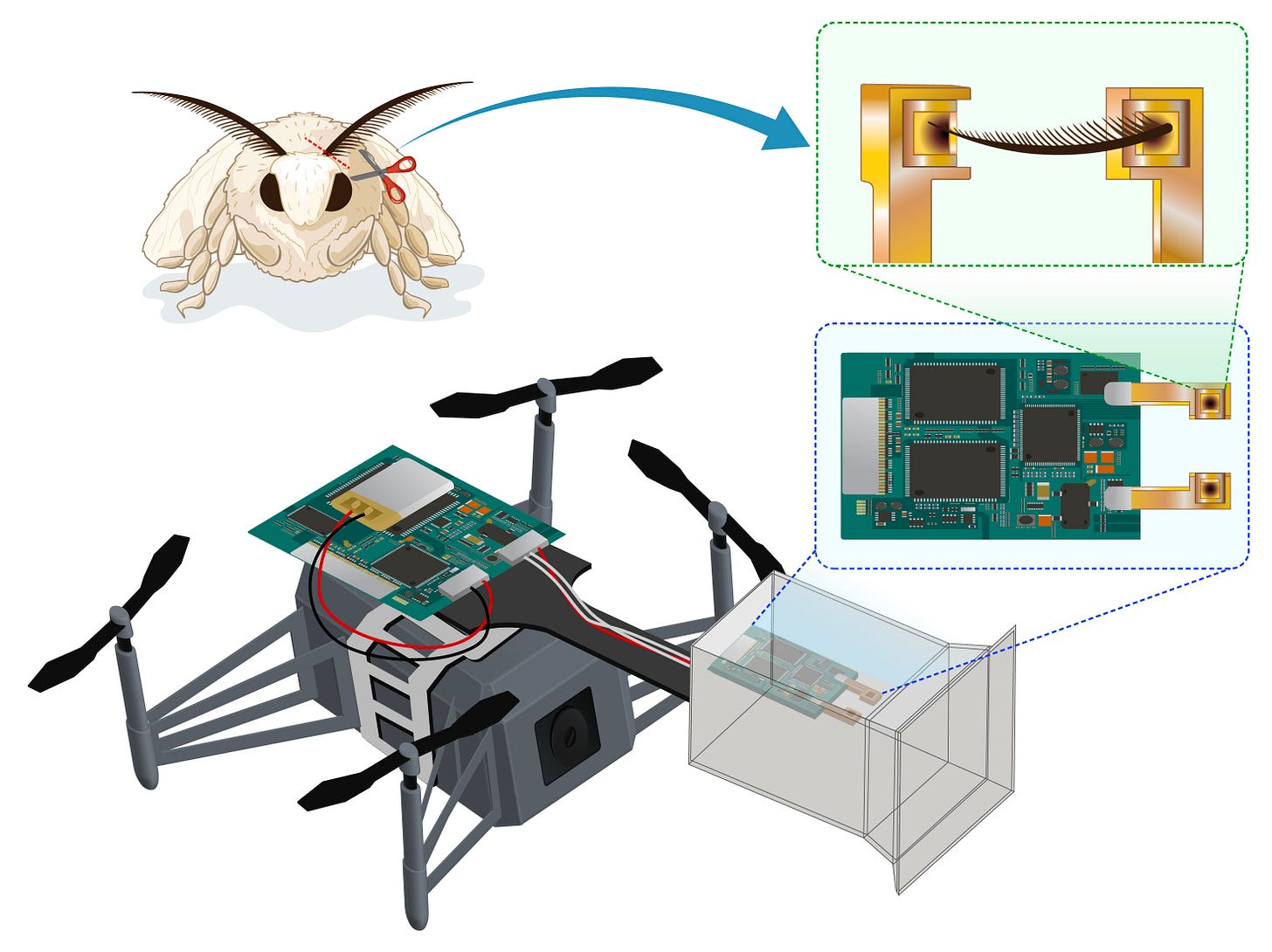
Then there’s the devices coming out. Some companies are trying to build electronic noses to help patients with anosmia. Loss of smell affects patients’ eating behavior, and their safety to detect poisonous gas, fire, and rotten food. Lawrence Livermore National Lab (my current employer and soon to be previous employer) recently announced a partnership with Canaery on a nose-computer interface to enhance animals’ ability to detect explosives. Canaery is attempting to digitize the olfactory signals from the brain using a microelectrode array implanted in rodents. This is to better improve chemical and biological detection. In Japan, a group just made a biohybrid drone that uses silkworm moth antennae to smell. The drone was implanted with the antennae from living moths, and the signal was measured using electroantennography (measuring the electrical signals from an insects antenna, part of insect electrophysiology). And there’s also ideas for making smell-based social media, like “Stinkygram” or “Nosebook.” Overall, I think this is a super cool emerging field.
What a future of smell diagnostics might look like?
So I want to end this post thinking about incorporating smell into medical diagnostics. I’m going to skip therapeutics (i.e. aromatherapy) because that’s something that’s been going on for centuries. The first thing I thought about when I thought smell diagnostics was actually breathalyzers. Beyond just detecting drunk drivers, breathalyzers are being explored to detect viruses and diseases. Noze is a company developing an advanced breathalyzer for point-of-care diagnostics for a variety of diseases, including metabolic diseases, gastroenterology, respiratory diseases, cardiovascular disorders, and cancer. Owlstone Medical is making a breathalyzer to act as a “Breath Biopsy” for all volatile organic compounds (VOCs) in your breath, which could be used for liver analysis and more. I am super interested because Owlstone Medical is going to release a VOC Atlas soon, which will allow others to explore the data they collected. We might even be able to find breath biomarkers for mental health disorders. There’s a smorgasbord of other companies out there, including Avelo and Deep Breath Intelligence that are still running today.
That was breath, but what about smell specifically? Olfactory function is already a part of clinical practice (which I’m now just learning about). There was a study on a Digital Scent Device 20, which provides 20 universal odors to measure your ability to smell. It correlated well with the standard Sniffin’ Sticks test (great name). Odor identification can be used as a measure of brain aging. In the future, odor identification might be a good biomarker to monitor dementia and other neurodegenerative diseases. And maybe it can be something widespread and done at home, with a device that can randomly generate odors to measure olfactory function.
I think the real future, however, will be the detection of odorants from sweat, skin, and other biospecimens. The simplest implementation would probably be a rapid test strip, but the detection proteins are olfactory membrane proteins. Maybe biomaterials that incorporate multiple olfactory receptors could be use as some advanced odor diagnostic. But the more advanced implementation would be akin to a wearable that can record your smell in real time. The “Oura ring of smells”, if you will. Odor monitoring could be use to measure both onset of disease and disease progression. This technique could also be super powerful for clinical trials, tracking whether drugs are actually preventing disease progression by real-time monitoring of smell. When full-body scanning for wellness, longevity, and health monitoring becomes more advanced, I could also imagine an odor technology also incorporated. We’ll need more understanding of smell biology and better technology, but I totally believe that odor and smell can become a digital biomarker measured in real time to track disease. And as it turns out, we’re not too far off. In 2017, Japanese company Konica Minolta released KunKun (sniff sniff in Japanese) to tell how smelly you are, so you didn’t have to ask your friends.
Maybe, in the future, KunKun will tell you if you have cancer, Parkinson’s or some other disease. Might never happen. But it might happen. Time will tell.









